The groundbreaking concept of engineered bacteria, initially developed to combat the parasitic infection amebiasis, has evolved into a revolutionary approach for treating nasopharyngeal carcinoma – by delivering cancer-fighting drugs with pinpoint accuracy.
In the intricate space behind our nasal cavity lies the nasopharynx, where a particularly challenging cancer – nasopharyngeal carcinoma – forms. Treatment for this cancer presents challenges due to its anatomical location, often requiring invasive procedures or chemotherapy that comes with debilitating side effects.
But imagine if treating this cancer could be as simple as using a nasal spray.
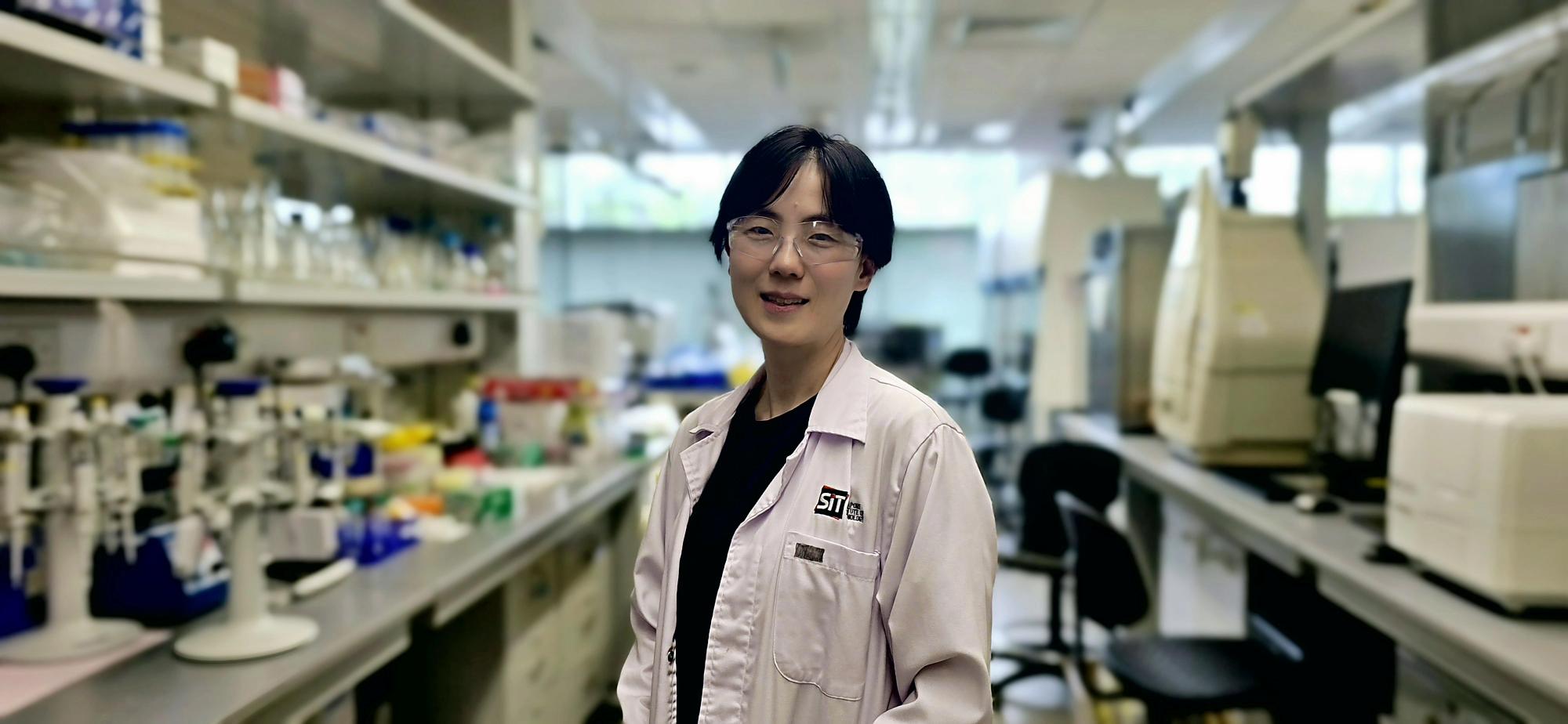
Associate Professor Hwang In Young led the development of a cancer-targeting bacterial therapy. (Photo: SIT)
This possibility is becoming increasingly viable, thanks to research led by Associate Professor Hwang In Young at the Singapore Institute of Technology (SIT). In 2024, she and her former colleagues at the NUS Synthetic Biology for Clinical and Technological Innovation (SynCTI and the Synthetic Biology Translational Research Programme at Yong Loo Lin School of Medicine at National University of Singapore (NUS), developed a therapy using engineered bacteria that can precisely target cancer cells while minimising harm to healthy tissue.
“We’re tapping into the vast reservoir of microorganisms already living in our bodies and turning it into a living medicine,” said A/Prof Hwang, who is now furthering the research at SIT’s Food, Chemical and Biotechnology Cluster. “They’re already involved in our normal physiological processes, so why not turn that into therapeutic modalities?”
The approach uses Lactobacillus plantarum, a beneficial probiotic that naturally binds to the surface of nasopharyngeal carcinoma cells. When engineered with a special anchor protein, these bacteria can carry anti-cancer drugs directly to the tumour site.
What makes this approach particularly promising is how it addresses one of chemotherapy’s biggest challenges: non-discriminate killing of healthy cells alongside cancerous ones.
“We use what is called ‘prodrugs’,” said A/Prof Hwang. “These are cancer-killing compounds attached to the surface of the bacteria in an inactive form until it reaches the cancer site. When the bacterium with prodrug binds to the cancer cells, prodrug is converted into its active form by the tumour microenvironment, triggering its cancer-killing effects precisely where needed.”
The research, published in Nature Communications in May 2024, showed promising results in laboratory settings using mice models, demonstrating tumour regression without the systemic toxicity associated with conventional chemotherapy.
By building on its original focus on combating amebiasis, this innovative bacterial therapy now holds tremendous potential for addressing both parasitic infections and complex cancers like nasopharyngeal carcinoma.
From Fighting Infections to Battling Cancer
The project was funded by the National Research Foundation through a joint programme with the Israel Science Foundation. The research grant was awarded while A/Prof Hwang was at the Department of Biochemistry, Yong Loo Lin School of Medicine, NUS, before she joined SIT.
Working with Israeli scientists, the team made strides in developing an approach that differed from conventional antibiotics.
The concept involved engineering a probiotic strain of bacteria to produce anti-parasitic peptides. When ingested by the amoeba, these peptides would be released inside the parasite, effectively transforming it into a self-destructive Trojan horse.
Unlike the broad-spectrum action of conventional antibiotics that kill bacteria directly, this approach repurposes bacteria as delivery vehicles that specifically target the parasite, releasing their therapeutic cargo only after being consumed by the pathogen, effectively turning the parasite into its own undoing.
But when COVID-19 disrupted international collaboration and laboratory work, the team had to pivot their research direction. Drawing on the platform they had already developed, the team began exploring how engineered bacteria could target cancer cells instead.
Chemotherapy Without the Side Effects
![The above diagram illustrates how the engineered bacteria target specific cancerous cells by delivering SN-38 prodrug by engineered Lp to NPC cells. [Image: Associate Prof Hwang In Young]](/sites/default/files/2025-05/Diagram%20engineered%20bacteria_0.png)
The above diagram illustrates how the engineered bacteria target specific cancerous cells through the delivery of SN-38 prodrug by engineered Lp to NPC cells. (SIT Photo: Hwang In Young)
The cancer-targeting approach works through a precise mechanism. The research team at NUS first screened various probiotic strains to identify those with the strongest natural affinity for binding to nasopharyngeal carcinoma cells. They then engineered these bacteria to express special anchor proteins on the surface, which were designed to hold prodrugs.
These anchor proteins act as attachment points for prodrugs, which remain inactive until they reach their destination. Once the bacteria bind to cancer cells, enzymes in the tumour microenvironment cleave the chemical linker, activating the drug directly at the tumour site for maximum efficacy.
What makes this platform so promising is its modularity, which has the potential to expand therapies beyond cancer. As this platform can facilitate intranasal delivery, it can also be used to access olfactory nerve endings found in the nasal cavity, which are connected directly to the brain. This access offers the potential to bypass the blood-brain barrier that often blocks therapeutic compounds from reaching neural tissues. This feature adds another layer of promise to the groundbreaking treatment strategy. “Cancer happens to be one target, but other diseases in this area can also be addressed,” said A/Prof Hwang.
The Gateway to Better Treatment Paradigms
This research exemplifies the growing field of synthetic biology, which applies engineering principles to biological systems for novel applications.
While safety and environmental concerns around the use of genetically modified organisms (GMOs) have initially been important considerations, regulatory frameworks are increasingly being established to guide their development and clinical evaluation.
Reflecting this progress, the United States’ Food and Drug Administration recently approved two microbiome-based drugs. Although these are not genetically modified, they could pave the way for engineered bacterial-based therapies to successfully navigate the established drug development and approval process.

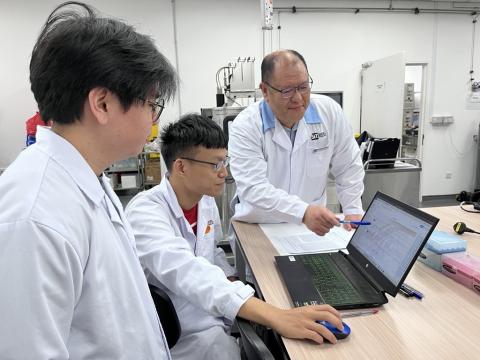
Associate Professor Hwang In Young is part of SIT’s growing faculty, driving innovation and collaboration across research fields such as bioengineering and materials characterisation. (Photo: SIT)
As Singapore positions itself to scale up in the ever-growing synthetic biology space, SIT has plans to tackle current research limitations by developing new bioproduction facilities at its Punggol campus. Features such as specialised labs and an Industrial Pilot Scales Space aim to provide students with hands-on experience in scaled-up production processes that simulate real-world manufacturing. Additionally, SIT's Centralised Analytical Testing (CAT) hub will foster innovation and collaboration across multiple research fields, supporting both SIT and industry in bioengineering, materials characterisation, and more.
“We’re just at the tip of the iceberg when it comes to discovering biomolecules from microorganisms that we can use for therapy or health in general,” said A/Prof Hwang. “It’s an exciting time to research this field because our capabilities are rapidly expanding.”
A/Prof Hwang is applying the same research skillsets to her current project in SIT, which explores the use of microbes to enhance the quality and precision of fermentation-based production of food ingredients – contributing to improved food security and sustainability in Singapore.














![[FA] SIT One SITizen Alumni Initiative_Web banner_1244px x 688px.jpg](/openhouse2025/sit-teaching-and-learning-academy/openhouse/centre-professional-communication/sites/default/files/2024-12/%5BFA%5D%20%20SIT%20One%20SITizen%20Alumni%20Initiative_Web%20banner_1244px%20x%20688px.jpg)


